Purpose of the Health Screening
This health screening is more comprehensive than the one conducted abroad for refugees. The objective of the health screening is to detect and begin treating any health condition. Refugees must be healthy in order to work. The clinic will collect all the necessary information to assist refugees in beginning medical care in the United States.
Also Read:- 4th Stimulus Check Update and Payment Status in 2022
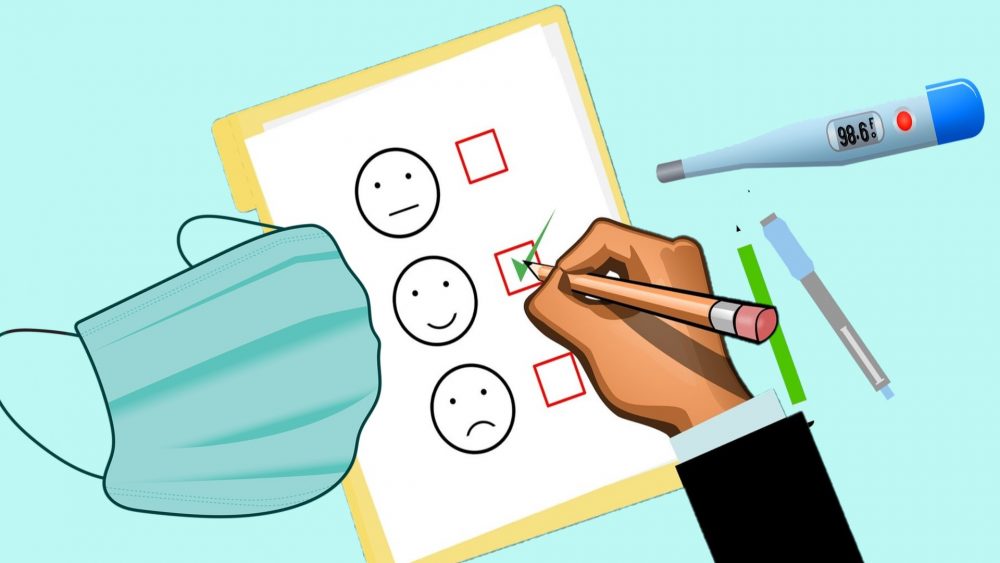
What to ExpectYour health screening includes:
- Medical history that involves an evaluation of overseas medical records
- Physical exam
- Screening for tuberculosis
- Immunizations
- Laboratory tests used for screening
- Screening for mental health, traumatic situations, and persecution (Refugees 16 years or older)
When a refugee arrives for an appointment, a healthcare provider will evaluate the refugee’s overseas medical and immunisation records. Then, a healthcare provider and other medical personnel will do an intake (first interview) and a physical examination. They will inquire about previous health issues and conduct a brief health education session. In addition, refugees will be required to provide blood, urine, and stool samples for testing of diseases such as tuberculosis, HIV, syphilis, hepatitis, anaemia, and parasites. In certain instances, refugees may also receive a tuberculin skin test and any necessary vaccinations. Blood samples from young children will be screened for lead. If a problem is detected during the health screening, the individual will be informed and referred to another clinic or specialist for further treatment. Refugees will receive copies of their health records following screening.
What They Should Bring to the Appointment
The International Organisation for Migration bag should be brought to the appointment by refugees (IOM). This bag holds the international health exam report. In addition to their passport or I-94 card, refugees should have their Medi-Cal card (if they have received it). If they are taking any medications, bring them with you.
Screening Tests for Common Diseases
What is a screening test?
The purpose of a screening test is to discover probable health issues or diseases in healthy individuals. To lower the risk of disease or to detect it early enough to treat it most effectively, early detection and lifestyle adjustments or surveillance are employed. Screening tests are not diagnostic, but they are used to identify a subset of the population that should undergo additional testing to evaluate the presence or absence of disease.
When is a screening test helpful?
The value of a screening test is in its capacity to uncover possible issues while minimising unclear, ambiguous, or confusing outcomes. Even while screening tests are not always 100 percent accurate, it is often more beneficial to have the screening tests at the prescribed intervals than to not have them at all. However, some screening tests, when administered to healthy individuals or when checking for extremely rare disorders, can cause more harm than good.
Some common screening tests
Consult your physician regarding the timing and frequency of all screening tests based on your age, general health, and medical history. The following are examples of typical screening procedures:
Cholesterol measurements
Cholesterol is a waxy molecule that is present throughout the body. It helps produce cell membranes, some hormones, and vitamin D. Cholesterol in the blood is derived from both dietary sources and liver synthesis. However, the liver creates all of the body’s cholesterol.
In the bloodstream, cholesterol and other fats are carried as spherical particles known as lipoproteins. Low-density lipoproteins (LDL), or “bad” cholesterol, and high-density lipoproteins (HDL), or “good” cholesterol, are the two most well-known lipoproteins.
A blood test is used for cholesterol checking. People with high cholesterol levels in a blood sample are at a greater risk for cardiovascular disease (CVD) compared to those with normal cholesterol levels. Those with high cholesterol can lessen their chance of developing heart disease, according to studies. It is essential to recognise, however, that people with normal cholesterol levels can nonetheless develop heart disease.
Faecal occult blood test
Microscopic analysis or chemical assays for haemoglobin (blood) in the stool reveal occult faecal blood. People with blood in their stool may have colorectal cancer-related malignant growths. The test requires the collection of three stool samples that are checked for blood under a microscope. Blood in a stool sample may be caused by noncancerous causes, including specific medications or foods, gastrointestinal bleeding, or haemorrhoids. Numerous groups, such as the American Cancer Society, recommend beginning testing at age 50.
Pap test (also called Pap smears)
Pap smears are samples of cells collected from a woman’s cervix to detect cellular abnormalities indicative of cervical cancer. The Pap smear is an important cancer screening test for sexually active women under the age of 65, as it can detect cancer at an early stage when no symptoms are present. It is vital to note that an “abnormal” Pap smear does not necessarily indicate that a woman has cervical cancer. Some organisations additionally advocate HPV (human papillomavirus) screening during the Pap smear for select populations.
Prostate specific antigen (PSA)
This blood test examines the levels of prostate specific antigen (PSA) in the bloodstream. Antigens are any compounds that stimulate an individual’s immune system. Prostate cancer can result in higher levels of prostate specific antigen. However, it is crucial to note that other benign prostate disorders, such as benign prostatic hyperplasia (BPH), a noncancerous enlargement of the prostate, may also boost PSA. The PSA test is not advised for all males, and its utility is the subject of substantial debate. Some organisations, like the United States Preventive Services Task Force (USPSTF), no longer advocate PSA screening. Before testing, always discuss the benefits and drawbacks of PSA screening with your physician. Excessive testing and procedures, unnecessary fees, and greatly increased anxiety are some of the disadvantages.
Mammography
After age 50, numerous organisations, including the USPSTF, suggest annual to biennial mammography screenings for breast cancer. This test is performed alongside a clinical breast exam.
Colonoscopy
Many organisations, including the USPSTF, advise screening for colon cancer or polyps at age 50, or earlier if there is a family history or other risk factors.
Diabetes or prediabetes
Regardless of weight, the American Diabetes Association (ADA) recommends screening all adults beginning at age 45 for diabetes or prediabetes. Additionally, individuals who are overweight or obese and have one or more additional diabetes risk factors should be screened for diabetes.
Consult your healthcare provider about all of these and other types of screening tests, based on your medical situation, as not all healthcare professionals agree on which screening tests should be performed and for which age groups.
Public Health Screening Programs
Screening for disease is one of the most fundamental instruments of contemporary public health and preventive medicine. In efforts to manage outbreaks of infectious diseases and target treatment for chronic disorders, screening programmes have a long and distinguished history. Women receiving prenatal care are typically tested for a full blood count and blood type, as well as diabetes and syphilis. Routinely, newborn children are screened for metabolic disorders and other conditions. Although the majority of these outcomes are uncommon, a positive test result activates measures that benefit both mother and child, and these efforts have led to significant health and well-being improvements.
Over the years that these screening programmes have been implemented, a large body of knowledge has been accumulated. In practise, gender inequality, racial discrimination, sexual taboos, and poverty impact the attitudes and beliefs of health system and public health decision makers, as well as patients, especially those who have lost faith that the health care system will treat them fairly. Consequently, if screening programmes are poorly conceived, managed, or implemented, they may result in questionable treatments and increase the vulnerability of groups and individuals.
This chapter provides background information on the vocabulary and generally accepted concepts that should drive public health screening activities, as well as the historical and social framework for implementing HIV screening programmes. The chapter opens with a discussion of screening as a public health paradigm, then analyses a number of historical instances of perinatal screening programmes in this context, and concludes with a summary of some of the challenges related with HIV testing in the United States
Screening Programs: A Model for Public Health
In the paradigm of public health, the terms “testing,” “screening,” “case finding,” “surveillance,” and “counselling” are crucial to comprehending what a screening programme entails. In the context of this report, testing refers to the administration of a test or measurement to a subset of individuals in order to diagnose an illness or medical condition. Individuals may be selected for testing based on clinical indications or risk factors suggesting the presence of the illness. Screening typically refers to the administration of a test to every member of a specified community. Screening is widely implemented for the goal of case finding, which is the identification of a previously unknown or undiagnosed ailment in apparently healthy or asymptomatic individuals and the provision of presymptomatic treatment to those so found. Occasionally, screening is performed for surveillance purposes: to track the incidence or prevalence of a disease in a specific population over time, or to compare the incidence or prevalence of a disease between populations. Surveillance is an essential public health activity for monitoring the effectiveness of preventative measures and allocating resources. Counselling is the process of communicating with individuals and their families about the nature, dangers, burden, and benefits of testing, as well as the significance of test results.
This paper focuses on HIV screening to identify and treat pregnant women for their own health and to avoid HIV transmission to their newborns, i.e. case discovery. Important endeavours, but not directly related to the committee’s function, include testing selected individuals and screening for surveillance purposes.
Principles of Public Health Screening
Experience with public health screening programmes has led to the development of a set of features of well-organised public health screening programmes (Wilson and Jungner, 1968). The following is the committee’s summary of the pertinent characteristics:
- The objectives of the screening programme should be clearly defined and demonstrated to be attainable.
- The natural history of the disorder should be thoroughly understood, and treatment or intervention for people who test positive should be broadly acknowledged by the scientific and medical community, supported by evidence that early intervention improves health outcomes.
- The screening test or measurement should differentiate between those who are likely to have the condition and those who are unlikely to have the disease. Tests can be evaluated based on their sensitivity (the proportion of actual instances where the test returns a positive result), specificity (the proportion of non-cases where the test returns a negative result), and positive predictive value (proportion of positive test results that are actual cases). When screening tests fail to identify the majority of people with an illness (false negatives) or identify significantly more people with the condition than actually have it, serious social, political, and economic problems sometimes occur (false positives).
- Those diagnosed with the ailment should have access to proper facilities for diagnosis and treatment, as well as an understanding of who will treat them. When screening programmes detect individuals with an illness but fail to give treatment, psychological suffering and social disturbance are likely to ensue.
- The affected population must find the test and potential interventions acceptable. For instance, a screening programme requiring all participants to have a spinal tap or offering pregnancy termination as the only choice may not be acceptable to certain communities. Concerns over the use of patient information or even the fundamental motivations (such as utilising the test as a means of discrimination to deny civil rights) may also render a programme inappropriate.
- The cost of case detection, diagnosis, and treatment or intervention should be economically balanced with the medical cost reductions that may emerge from the screening programme. Screening programmes are not required to be cost-effective, but their costs must be acceptable in relation to the anticipated benefits and other public health programme opportunities.
Various legal and ethical principles should apply to public health screening initiatives as well (Faden et al., 1991). As a general rule, the least burdensome (from a legal and ethical standpoint) strategy that satisfies public health objectives should always be chosen.
First and foremost, programmes must comply with the United States and state constitutions, common law, and legislative obligations. Targeted screening programmes, for instance, must avoid concerns associated with the denial of equal protection when testing specific groups. In addition, the means to attain otherwise acceptable social goals must be tightly circumscribed to prevent interference with the practice of other vital liberties, such as privacy. In addition, screening programmes must adhere to existing legal obligations including informed consent and confidentiality, duty to treat, and standards of professional negligence (Faden et al., 1991).
Additionally, non-legal moral issues must be taken into account. These issues are guided by three broad tenets: beneficence, autonomy, and social justice. Beneficence refers to the necessity to weigh the advantages of public health initiatives (mostly illness prevention) against their disadvantages (which could be physical or involve the loss of privacy or autonomy). Respect for autonomy highlights the significance of personal freedom and choice in both political life and personal decisions. Justice pertains to the equitable allocation of public health programme benefits and costs. None of these principles can be continuously viewed as more significant than the others, but the degree to which they are satisfied must always be balanced (Faden et al., 1991)